


We are most convenient to patients from Westwood, Dedham, Canton, Norwood, and Needham MA. Additionally we serve Medfield, Dover, and the entire Boston area.
People generally think of teeth as being white. But tooth enamel can be many different shades. Over time, tooth enamel can change color or become stained. There are many reasons why teeth become discolored:
If your teeth are discolored, tooth whitening may help. "Whitening" is any process that can make teeth look whiter. It may be safely done at home or in a dental office.
Tooth-whitening options range from gentle surface whiteners to stronger ones that can also remove deeper stains. There are many different types of tooth whitening products. They fall into three main types:
Whitening toothpastes help remove stains on the surface of your teeth. They are the gentlest kind of whiteners. Since they work using polishing action rather than chemicals, they usually do not have side effects. However, they do not get teeth as white as chemical products. Whitening toothpastes can lighten teeth a little bit at a time, over days or weeks, and can be purchased over the counter.
Home-use whiteners come from your us or are sold over the counter. They can be applied with trays, strips, a rinse, or a brush. They usually contain a chemical called peroxide, which gets below the surface to lighten tooth enamel. Home-use whiteners are meant to be used over days or weeks. It is best to consult your us before whitening your teeth.
We may make special whitening trays for your upper and lower teeth. You put the whitening gel in the trays and wear them for short times during the day or overnight. We will tell you how long to wear them - if you wear the trays for too long, the peroxide in the gel can irritate your teeth.
We offer in-office whitening using the Philips ZOOM! laser whitening system - your teeth can be up to 8 shades whiter after one 60 minute treatment. Click here for more information on ZOOM! teeth whitening.
For a few days after treatment, your teeth may be sensitive to very hot or cold temperatures. Whitening may also irritate the gums for a short time. If the side effects do not go away after a few days, see your dentist.
To avoid harming your teeth and gums, always follow the product directions and any instructions from your dentist. If your teeth become very sensitive or you get sores in your mouth, stop using in-home products and call your dentist.
There is such a thing as too much whitening. Do not use whitening products for longer than advised in the product directions or by your dentist. Overwhitening can cause severe discomfort to your teeth and gums. Too much whitening can even harm your tooth enamel.
Tooth whitening is not a good choice for all people. If your gums have pulled away from the teeth in some places, whitening may irritate these areas. If you have tooth decay or gum disease, your dentist may recommend that these be treated before whitening. Also, the color of fillings, crowns, and some stains cannot be changed by tooth whitening.
So talk to your dentist about tooth whitening before you begin. He or she will do an oral exam to find out if tooth whitening is right for you.
Newly whitened teeth may stain more easily. To keep your teeth white as long as possible, avoid tobacco and stain-causing food and drinks for several days after whitening. Keep in mind that teeth usually return to their original shade over time. But if you steer clear of tobacco and large amounts of stain-causing food and drinks, your teeth may stay bright for several years.
As discussed on About the Practice, as a small child Dr. Dan underwent a four hour root canal procedure with no anesthetic. Since that day, he vowed to never let that happen to anyone else, and dedicated himself to painless, gentle dentistry. Every aspect of our practice has been considered with your comfort in mind, and Dr. Dan will do his utmost to put your mind at ease.
Tooth decay is a disease that damages and breaks down teeth. A tooth has a hard outer layer (enamel), a middle layer (dentin) and a center (pulp). The more layers affected by decay, the worse the damage.
If tooth decay is not treated, it can lead to pain, the spread of infection, loss of teeth and loss of self-confidence. An abscess (pus-filled sac) from a cavity can cause serious or even life-threatening infections when not properly treated. It is much simpler and more affordable to prevent tooth decay than to repair or replace a decayed tooth.
Your teeth are covered by a sticky film of bacteria called plaque. After a meal or snack, the bacteria turn the sugars in foods and drinks into acid. The acid attacks the tooth enamel. The acid eats away at the tooth and can cause decay. A hole called a cavity can form.
People of all ages can get tooth decay. Your risk may increase if you:
Tooth decay can be prevented if you:
Treatment of decay depends on how early the decay is caught. Before cavities form, fluoride treatments may solve the problem. If you have a cavity, you'll need a filling. A large cavity may need a crown to replace the decayed part of the tooth. If the center (pulp) of your tooth is involved, root canal treatment may be your last chance to save the tooth. Finally, a badly damaged tooth might have to be pulled and replaced. Your dentist will discuss options and plan the best way to get your mouth healthy again.
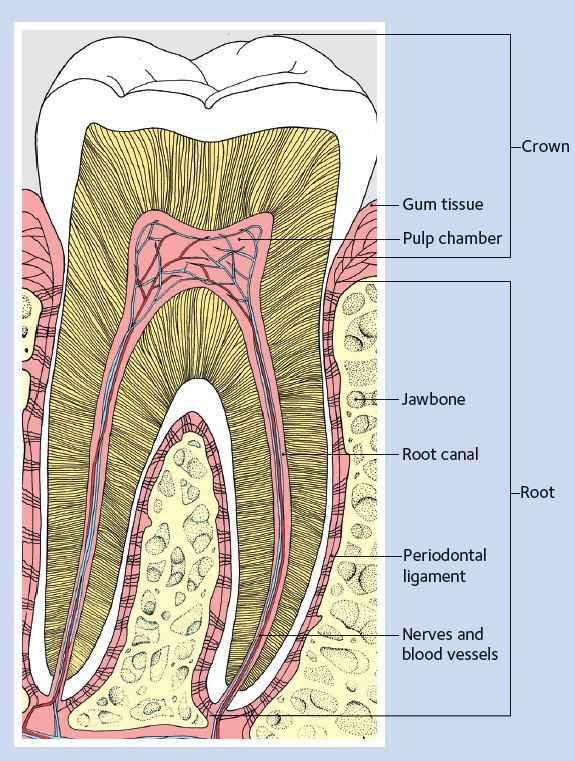
Healthy tooth
It's easy to keep your teeth and gums in good health. A simple routine of daily teeth cleaning, good eating habits and regular dental visits can help prevent tooth decay (cavities) and gum disease.
Your teeth are covered with a sticky film of bacteria called plaque. If you brush twice a day and floss once a day, you can remove most of the harmful plaque and bacteria. But if plaque stays on the teeth, it will eventually harden into tartar. It is harder to brush and floss when tartar builds up near the gumline.
Brush twice a day with a fluoride toothpaste to help prevent tooth decay. Select a toothbrush that feels comfortable in your hand and in your mouth. Replace your toothbrush every three or four months, or sooner if the bristles become frayed. If you have hand, arm, or shoulder problems that limit movement, you may find a powered toothbrush easier to use.
Even if you brush twice a day, there are places your toothbrush bristles can't reach. Flossing removes plaque and food particles from between teeth and under the gumline. A simple routine of daily teeth cleaning, good eating habits and regular dental visits can help prevent tooth decay (cavities) and gum disease.
If you have trouble handling floss, you may wish to try a floss holder or another type of interdental cleaning aid. Interdental cleaners include narrow brushes, picks, or sticks used to remove plaque from between teeth. Your dentist or hygienist can tell you how to use these special cleaners.
Our current recommendation is the Sonicare Diamondclean toothbrush, and Colgate toothpaste.
There can be many causes for tooth pain, including dental decay, an injury or infection. If you have tooth pain, read on to find your symptoms, possible causes and treatment options. If you have ongoing pain or discomfort, please contact us.
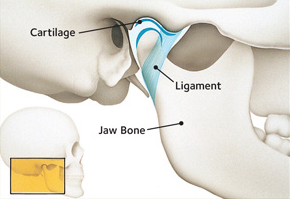
Do you have frequent headaches, earaches, tender jaw muscles or a dull, aching facial pain? Does your jaw lock or stray to one side when you open your mouth? These aches and pains may be related to the jaw joint, called the temporomandibular joint or "TMJ," and the muscles that work to move the joint. These painful conditions are often called "TMD" for temporomandibular disorders.
A TMD is a condition, not a specific disease. Temporomandibular disorders can have many different signs and symptoms, from mild to severe. Some patients may have symptoms but are still able to function fully. TMDs appear to be more common in women. Specific symptoms may include:
Several conditions may be linked with TMD. This often makes it difficult to pinpoint the cause of a particular case of TMD. Related conditions may include:
To determine how best to treat your condition, a complete evaluation is recommended. Your dentist may check the joints and muscles for tenderness, clicking, popping or difficulty moving. Your complete medical history may be reviewed, so it is important to keep your dental office record up-to-date. Your dentist may take X-rays and may make a model of your teeth to see how your bite fits together. Your dentist may also request specialized X-rays of the TM joints.
The joints and muscles on each side of your jaw help open and close the mouth. These joints move in many different directions. They allow you to chew, talk and swallow.
The two temporomandibular joints are among the most complex joints in the body. They work together in a delicate balance with muscles, ligaments, cartilage and your jaw bones. When a problem prevents these parts from working together properly, pain may result.
For some patients, the disorders may disappear by themselves; for others, they may come and go, or may worsen over time. TMD disorders are often managed, rather than cured. Your general dentist may recommend treatment, or he or she may refer you to a physician or dental specialist.
There are several ways TMD may be managed. The success of the treatment often depends upon you and your dentist working together to find what works to relieve your symptoms.
Treatment may involve a series of steps. The step-by-step plan allows you to try simple treatment before moving on to more involved treatment. Experts generally recommend a "less is often best" approach to treating TMJ disorders.
The following self-care practices may be recommended:
If necessary, your dentist may recommend the following to relieve your symptoms:
In some cases, your dentist may recommend fixing an uneven bite by adjusting or reshaping some teeth. Orthodontic treatment may also be recommended.
Dry mouth - also called xerostomia - results from an inadequate flow of saliva. It is not a disease, but a symptom of a medical disorder or a side effect of certain medications, such as antihistamines, decongestants, pain killers, diuretics and many others.
Saliva is the mouth's primary defense against tooth decay and maintains the health of the soft and hard tissues in the mouth. Saliva washes away food and other debris, neutralizes acids produced by bacteria in the mouth and provides disease-fighting substances throughout the mouth, offering first-line protection against microbial invasion or overgrowth that might lead to disease.
Some of the common problems associated with dry mouth include a constant sore throat, burning sensation, trouble speaking, difficulty swallowing, hoarseness or dry nasal passages. In some cases, dry mouth can be an indicator of Sjögren's (pronounced SHOW-grins) syndrome. Sjögren's syndrome is a chronic autoimmune disorder in which the body's immune system mistakenly attacks its own moisture-producing glands, the tear-secreting and salivary glands as well as other organs.
Without saliva, extensive tooth decay can also occur. Your dentist can recommend various methods to restore moisture. Sugar-free candy or gum stimulates saliva flow, and moisture can be replaced by using artificial saliva and oral rinses.
For more information, visit the Sjögren's Syndrome Foundation.
Bad breath happens. If you've ever gotten that not-so-fresh feeling on a date, at a job interview or just talking with friends, you're not alone. Studies show that 50 percent of adults have had bad breath, or halitosis, at some point in their lives.
There are a number of reasons you might have dragon breath. While many causes are harmless, bad breath can sometimes be a sign of something more serious.
Bad breath can happen anytime thanks to the hundreds of types of bad breath-causing bacteria that naturally lives in your mouth. Your mouth also acts like a natural hothouse that allows these bacteria to grow. When you eat, bacteria feed on the food left in your mouth and leaves a foul-smelling waste product behind.
Feeling parched? Your mouth might not be making enough saliva. Saliva is important because it works around the clock to wash out your mouth. If you don't have enough, your mouth isn't being cleaned as much as it should be. Dry mouth can be caused by certain medications, salivary gland problems or by simply breathing through your mouth.
Bad breath that just won't go away or a constant bad taste in your mouth can be a warning sign of advanced gum disease, which is caused by a sticky, cavity-causing bacteria called plaque.
Garlic, onions, coffee... The list of breath-offending foods is long, and what you eat affects the air you exhale.
Smoking stains your teeth, gives you bad breath and puts you at risk for a host of health problems. Tobacco reduces your ability to taste foods and irritates gum tissues. Tobacco users are more likely to suffer from gum disease. Since smoking also affects your sense of smell, smokers may not be aware of how their breath smells.
Mouth infections can cause bad breath. However, if your dentist has ruled out other causes and you brush and floss every day, your bad breath could be the result of another problem, such as a sinus condition, gastric reflux, diabetes, liver or kidney disease. In this case, see your healthcare provider.
Brush twice a day and clean between your teeth daily with floss to get rid of all that bacteria that's causing your bad breath.
Don't forget about your tongue when you're taking care of your teeth. If you stick out your tongue and look way back, you'll see a white or brown coating. That's where most of bad breath bacteria can be found. Use a toothbrush or a tongue scraper to clear them out.
Over-the-counter mouthwashes can help kill bacteria or neutralize and temporarily mask bad breath. It's only a temporary solution, however. The longer you wait to brush and floss away food in your mouth, the more likely your breath will offend.
If you wear removable dentures, take them out at night, and clean them thoroughly before using them again the next morning.
To get more saliva moving in your mouth, try eating healthy foods that require a lot of chewing, like carrots or apples. You can also try chewing sugar-free gum or sucking on sugar-free candies. Your dentist may also recommend artificial saliva.
Giving up this dangerous habit is good for your body in many ways. Not only will you have better breath, you'll have a better quality of life.
If you're concerned about what's causing your bad breath, make an appointment to see your dentist. Regular checkups allow your dentist to detect any problems such as gum disease or dry mouth and stop them before they become more serious. If your dentist determines your mouth is healthy, you may be referred to your primary care doctor.
Periodontal (gum) disease is an infection. It affects the tissues and bone that support the teeth. Healthy gum tissue fits like a cuff around each tooth. When someone has periodontal disease, the gum tissue pulls away from the tooth. As the disease gets worse, the tissue and bone that support the tooth are damaged. Over time, teeth may fall out or need to be removed. Treating periodontal disease in the early stages can help prevent tooth loss.
Periodontal disease has been linked to some other diseases. People with diabetes or heart disease are more likely to get periodontal disease. Strokes and high stress also may be related to periodontal disease.
Periodontal disease is caused by plaque, a sticky film that is always forming on your teeth. Plaque contains bacteria that can irritate and inflame the gums.
Inflamed gums can pull away from the teeth and form spaces called "pockets." These pockets collect more bacteria. If the infected pockets are not treated, the gum disease can get worse.
You can have periodontal disease and not notice any of these warning signs. That is why regular dental checkups are very important.
Anyone can get periodontal disease. These things can increase the risk:
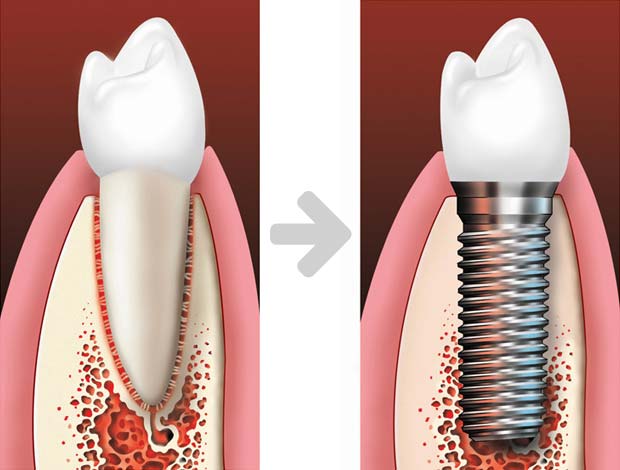
Many kinds of dental implants are available. Treatment can take one day, several months, or somewhere in between, and usually involves three basic steps.
Your dentist will carefully locate where the implant should be placed, using x-rays or other pictures. Then the dentist surgically places the implant into the jawbone.
What makes an implant so strong is that the jawbone grows around it and holds it in place. This process, called osseointegration (OSS-e-o-in-te-GRAY-shun), can take several months before the implant is completely integrated into the bone. Then the patient can get the permanent replacement tooth or teeth. In many cases, the implant and temporary replacement teeth can be placed in one visit.
Single tooth crowns, implant-supported bridges and dentures are all custom-made to look like natural teeth and to fit your mouth. The replacement tooth or teeth are attached to the implant post(s).

The single tooth implant replaces the missing tooth's roots. A single tooth implant is a stand-alone unit and does not involve treating the teeth next to it. If you are missing one or more teeth, there are many reasons why you should replace them:
Dental implants can be used to support a bridge when several teeth are missing. The implant-supported bridge replaces the lost natural teeth and some of the tooth roots. Unlike traditional bridges, an implant-supported bridge does not need support from the teeth next to it.

If you are missing all of your teeth, an implant-supported denture can replace the missing teeth and some of the tooth roots. Because the dental implants integrate (or "fuse") with the jawbone, an implant-supported denture tends to be comfortable and stable, allowing you to bite and chew naturally.
If you are missing all of your teeth, an implant-supported denture can replace the missing teeth and some of the tooth roots. Because the dental implants integrate (or "fuse") with the jawbone, an implant-supported denture tends to be comfortable and stable, allowing you to bite and chew naturally.



With age comes wisdom. Specifically, wisdom teeth.
Your mouth goes through many changes in your lifetime. One major dental milestone that usually takes place between the ages of 17 and 21 is the appearance of your third molars. Historically, these teeth have been called wisdom teeth because they come through at a more mature age.
When they come through correctly, healthy wisdom teeth can help you chew. It's normal to feel a little discomfort when your wisdom teeth appear, but if you have pain, see your dentist immediately.
Wisdom teeth can lead to problems if there isn’t enough space for them to surface or they come through in the wrong position. If your dentist says your wisdom teeth are impacted, he or she means they are trapped in your jaw or under your gums.
As your wisdom teeth make their way through your gums, your dentist will be monitoring your mouth for signs of the following:
Every patient is unique, but in general, wisdom teeth may need to be removed when there is evidence of changes in the mouth such as:
Your dentist may also recommend removal of wisdom teeth as part of treatment for braces or other dental care.
Before making any decisions, your dentist will examine your mouth and take an x-ray. Together, you and your dentist can discuss the best course of treatment.
Wisdom teeth that are not removed should continue to be monitored because the potential for developing problems later on still exists. As people age, they are at greater risk for health problems—and that includes potential problems with their wisdom teeth. Be sure to, floss around your wisdom teeth and visit your dentist regularly. Regular dental visits allow your dentist to evaluate your wisdom teeth and your overall dental health.
The linea alba (Latin for white line) is a term used in dentistry to describe a horizontal streak on the inner surface of the cheek, level with the biting plane. It is a common finding and most likely associated with pressure, frictional irritation, or sucking trauma from the facial surfaces of the teeth. It may be found in individuals who chew tobacco, and may be mistaken for a lesion requiring treatment.
Leukoplakia (loo-koh-PLAY-kee-ah) is a white or gray patch that develops anywhere on the inside of the mouth. It is caused by excess cell growth of the lining of the mouth. It is often a response to chronic irritation, such as smoking or smokeless tobacco (snuff, chewing tobacco), certain foods, cheek biting, irregular dental restorations or broken teeth. In some instances, a cause cannot be determined. Leukoplakia patches develop slowly over a period of time. The patch may eventually become rough. It typically is not sensitive or painful.

Leukoplakia generally is harmless, but there is a risk that it can become cancerous. To be certain that a spot or sore is not a threat, your dentist may do a biopsy to determine if any potentially dangerous cells are present. If the leukoplakia is sensitive, cancer must be ruled out by biopsy.
You know smoking is bad for your health, so it should be no surprise that cigarettes and chewing tobacco are also harmful to your oral health. For one, tobacco products can cause bad breath, but that’s only the beginning.
Smokeless tobacco goes by many names, such as chewing tobacco, oral tobacco, spitting tobacco, dip, chew, and snuff.
Some of the side effects include:
If more than 3 of the above questions pertain to you, it would be best to schedule a consultation appointment where we can discuss your case and examine your concerns.
Reach Doctor Dan at the office at (781) 733-9378 or contact him via email. Simply paste your question into the subject line and body of the email along with your name and phone number. Providing your contact information will allow multiple or extensive questions to be answered on a more personal level.


Includes a cleaning, comprehensive exam, oral cancer screening, perio charting, and needed x-rays.
*Patients with periodontal disease may require additional visits which may include additional cost.
** For new patients only without insurance
Emergency line, 24 hours/day
781-686-3284
Appointments, office and insurance
office@dentalartsofwestwood.com